Starving Cancer: Dr. Thomas Seyfried’s Metabolic Therapy for Glioblastoma
Introduction
“Cancer is primarily a disease of energy metabolism.”
— Dr. Thomas N. Seyfried, Professor of Biology, Boston College
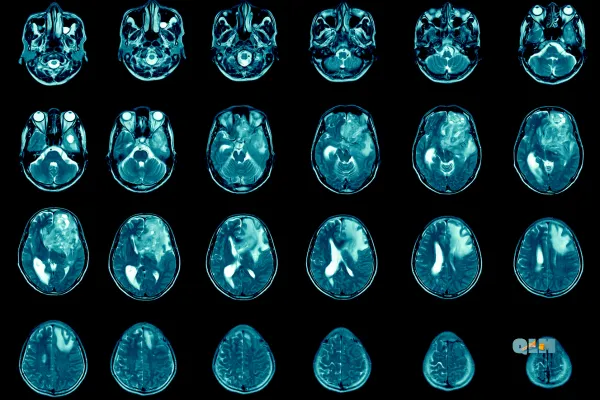
Glioblastoma multiforme (GBM) is one of the deadliest forms of brain cancer. Fast-growing, highly invasive, and notoriously resistant to treatment, glioblastoma carries a median survival time of just 12 to 15 months despite aggressive therapy with surgery, radiation, and chemotherapy [Cancer].
But a growing number of researchers are challenging the traditional view of glioblastoma as simply a genetic disease. One of the most vocal and well-respected among them is Dr. Thomas Seyfried, a professor and researcher who argues that GBM—and many other cancers—are primarily metabolic disorders rooted in dysfunctional mitochondrial energy production.
Seyfried’s research builds on the century-old work of Nobel laureate Otto Warburg, who first proposed that cancer cells ferment glucose even when oxygen is available—a process known as the Warburg Effect. Seyfried takes this a step further, suggesting that glioblastoma can be managed—if not reversed—by targeting the metabolic environment that cancer cells depend on to survive and spread.
This article explores:
What glioblastoma is and why it’s so lethal
The metabolic vulnerabilities of cancer cells
Seyfried’s ketogenic and press-pulse approach to treatment
The evidence, the controversy, and what this could mean for the future of brain cancer therapy
🎧 Listen to the Episode: Can We Starve Brain Cancer?
Glioblastoma is one of the most aggressive cancers known—but it may have a weakness. In this episode of The Health Pulse, we break down Dr. Thomas Seyfried’s metabolic therapy approach, why GBM cells depend on glucose and glutamine, and how diet and targeted interventions could give patients more time and better quality of life.
▶️ Click play below to listen, or keep reading to explore how the metabolic theory of cancer could transform treatment for glioblastoma and beyond.
What Is Glioblastoma?
Glioblastoma multiforme (GBM) is the most aggressive and common form of malignant brain tumor in adults. Arising from glial cells—specifically astrocytes—glioblastomas grow rapidly, infiltrate surrounding brain tissue, and resist most conventional treatments.
Key Characteristics of GBM:
Fast-growing and invasive: GBM spreads tentacle-like projections deep into the brain, making surgical removal nearly impossible without damaging healthy tissue.
Highly heterogeneous: These tumors contain a mix of cell types and mutations, making them adaptable and hard to target with a single drug or therapy.
Blood-brain barrier challenges: Many chemotherapy agents can’t effectively penetrate the brain, reducing their impact on tumor cells.
Prognosis and Standard Treatment
Despite advances in neurosurgery and oncology, the standard of care includes:
Surgical resection (if feasible)
Radiation therapy
Temozolomide chemotherapy
Palliative care and symptom management
Unfortunately, even with aggressive treatment, the median survival remains 12–15 months, and five-year survival is less than 10% [NIH].
Why GBM Is So Difficult to Cure
GBM’s resistance lies not only in its physical location and infiltration but also in its biological behavior:
It thrives in inflammatory, hypoxic (low-oxygen), and high-glucose environments
It recruits its own blood supply (angiogenesis)
It bypasses cell death mechanisms (apoptosis)
It evades the immune system
These properties have led researchers like Dr. Seyfried to question whether targeting GBM’s fuel source, rather than just its DNA mutations, might offer a more effective therapeutic path.
Bottom line:
Glioblastoma is aggressive, adaptable, and nearly impossible to cure with conventional therapy alone. Its survival depends heavily on its metabolic environment—which may be its greatest weakness.
The Warburg Effect: Cancer’s Metabolic Weakness
In the 1920s, Nobel Prize-winning scientist Dr. Otto Warburg made a discovery that would reshape cancer biology: cancer cells generate energy through fermentation, even when oxygen is available. This phenomenon, now known as the Warburg Effect, puzzled scientists for decades.
Normal vs. Cancer Cell Metabolism
Healthy cells typically produce energy through:
Glycolysis (sugar → small amount of ATP)
Followed by oxidative phosphorylation (OxPhos) in the mitochondria (→ lots of ATP)
Cancer cells, by contrast, rely heavily on:
Aerobic glycolysis → sugar is fermented to lactate
Even in the presence of oxygen
Less efficient, but fast and supports rapid growth
Why This Matters for Glioblastoma
Glioblastoma cells have been shown to:
Consume massive amounts of glucose
Thrive in hypoxic (low-oxygen) environments
Show damaged or dysfunctional mitochondria, impairing their ability to use fat or ketones for fuel [3]
This creates a metabolic vulnerability:
Take away glucose, and you starve the tumor.
It’s Not Just About Genes
While mainstream cancer therapy focuses heavily on genetic mutations, Dr. Thomas Seyfried and others argue that many of these mutations are secondary to the real issue: mitochondrial dysfunction.
In this view, cancer is primarily a metabolic disease, and the Warburg Effect is both a symptom and survival strategy of a cell that has lost normal energy production.
Glioblastoma’s reliance on glucose and glutamine for survival makes it uniquely vulnerable to therapies that restrict these fuels. This is where Dr. Seyfried’s metabolic approach begins.
Seyfried’s Metabolic Theory of Cancer
While most oncologists still view cancer primarily through the lens of genetic mutations, Dr. Thomas N. Seyfried—a professor of biology at Boston College—has proposed a different paradigm:
Cancer begins with damaged mitochondria and disordered energy metabolism.
In his influential book, Cancer as a Metabolic Disease, Seyfried argues that the defining feature of cancer cells isn't their DNA mutations—it’s their inability to produce energy normally through oxidative phosphorylation (OxPhos). Instead, cancer cells are forced to rely on fermentation of glucose and glutamine to survive and grow.
Mitochondrial Dysfunction Comes First
According to Seyfried:
Mitochondrial damage disrupts normal cell signaling and energy production
This leads to compensatory fermentation (glycolysis)
Only then do genetic mutations accumulate as a downstream effect
This flips the mainstream model on its head.
Glucose and Glutamine: Cancer’s Two Fuels
In the Seyfried model, cancer cells are metabolically inflexible. They thrive on:
Glucose – processed through glycolysis to lactate
Glutamine – used for substrate-level phosphorylation in the mitochondria
By targeting both fuels, it may be possible to induce a metabolic crisis in tumor cells—leading to cell death without harming normal tissue, which can switch to using fat and ketones for energy.
Press-Pulse Strategy: A Novel Therapeutic Framework
Seyfried proposes a two-part intervention called Press-Pulse Therapy, designed to metabolically “trap” cancer cells:
Press = Chronic pressure through a ketogenic diet (low glucose, high ketones)
Pulse = Acute interventions, like fasting, hyperbaric oxygen, or glutamine inhibitors to deliver metabolic “shocks”
Together, these strategies exploit the metabolic inflexibility of cancer cells, pushing them toward apoptosis (programmed cell death) while sparing healthy cells [NIH]
Therapeutic Strategies: Ketosis, Glutamine Restriction, and More
If glioblastoma thrives on glucose and glutamine, then denying it access to those fuels may weaken or kill the tumor cells. That’s the premise behind Seyfried’s metabolic therapy approach, which includes:
Ketogenic Diet (Keto for Cancer)
A ketogenic diet is high in fat, moderate in protein, and very low in carbohydrates—designed to drastically lower blood glucose while elevating ketone bodies like beta-hydroxybutyrate (BHB).
Normal brain cells can use ketones efficiently.
Glioblastoma cells, with defective mitochondria, cannot.
Studies have shown that therapeutic ketosis can slow tumor growth, reduce inflammation, and sensitize tumors to other treatments [Nutrients].
Glutamine Restriction
While glucose restriction is achievable through diet, glutamine—the second major fuel for glioblastoma—is more difficult to control, as it’s synthesized and circulated throughout the body.
Seyfried and colleagues propose:
Fasting protocols to lower glutamine availability
Inhibitors like DON (6-Diazo-5-oxo-L-norleucine) to block glutamine metabolism
Time-restricted eating and caloric restriction to lower systemic growth signals
Some combination of glucose and glutamine restriction appears necessary to fully suppress glioblastoma metabolism [Nutrition and Metabolism]
Hyperbaric Oxygen Therapy (HBOT)
Tumor cells thrive in hypoxic (low-oxygen) environments, where they rely on glycolysis.
HBOT increases oxygen saturation in the blood and tissues, disrupting this environment and enhancing oxidative stress in cancer cells—particularly when combined with ketosis.
Early animal studies suggest that HBOT synergizes with ketogenic therapy to slow tumor progression [Signal Transduction and Targeted Therapy]
Targeted Supplements and Lab Monitoring
To support mitochondrial health and therapy, Seyfried’s approach may include:
CoQ10, magnesium, B vitamins, L-carnitine
Tracking glucose:ketone index (GKI) to measure metabolic status
Monitoring CRP, lactate, insulin, and beta-hydroxybutyrate
Bottom line:
Seyfried’s protocol combines ketosis, glutamine restriction, oxygen therapy, and fasting into a coherent strategy to weaken glioblastoma metabolically—without the toxicity of traditional chemotherapy.
Challenges, Controversies, and Clinical Applications
While Dr. Seyfried’s metabolic therapy model offers a compelling and science-backed alternative to conventional oncology, it hasn’t yet been widely adopted in clinical settings. That’s due to a mix of scientific, institutional, and practical challenges.
Challenges and Limitations
Lack of Large-Scale Clinical Trials
Metabolic therapies—like ketogenic diets and glutamine inhibition—are still in the early stages of research. While preclinical animal models and individual case reports show promise, randomized controlled trials in humans are limited.
Integration With Standard Care
Most oncologists rely on surgery, radiation, and chemotherapy—approaches backed by decades of trial data. Integrating metabolic therapies into these regimens remains controversial due to:
Concerns about nutrient deficiencies
Fear of delaying standard treatment
Lack of insurance reimbursement or institutional protocols
GBM’s Complexity
Even with metabolic restriction, glioblastomas are highly adaptable. They can shift fuel sources or hijack surrounding support cells (like astrocytes) to survive.
This means metabolic therapy is not a silver bullet, but potentially a powerful adjunct to standard care.
Clinical Case Reports and Emerging Data
Despite the challenges, there are case studies of patients with glioblastoma who experienced extended survival, tumor shrinkage, or improved quality of life using metabolic approaches—often alongside standard treatments.
For example:
A 2010 case study published in Nutrition & Metabolism reported stable disease in a GBM patient using a calorie-restricted ketogenic diet [NIH]
New pilot trials are exploring combinations of keto, hyperbaric oxygen, and immunotherapy.
As interest grows among patients, more clinicians and researchers are beginning to explore these interventions—especially for cases with limited options.
Patient-Led Demand
Many patients and caregivers are now driving the demand for metabolic therapies. Online communities, integrative oncologists, and platforms like the Metabolic Health Summit have created awareness beyond academic circles.
While still experimental, these approaches often give patients:
A sense of control
Reduced treatment-related side effects
Improved metabolic health and immune support
Bottom line:
Metabolic therapy for glioblastoma is not yet mainstream—but it’s no longer fringe. With growing scientific interest and patient advocacy, it may become a vital part of personalized, integrative cancer care.
Conclusion: Rethinking Glioblastoma from the Inside Out
Glioblastoma remains one of the most aggressive and fatal forms of cancer. Despite surgery, chemotherapy, and radiation, outcomes haven’t improved much in decades. But a growing body of research—led by Dr. Thomas Seyfried and others—suggests a paradigm shift is underway.
Instead of focusing solely on genetic mutations, metabolic therapy targets the core survival mechanisms of glioblastoma: its dependence on glucose and glutamine, and its inability to adapt to ketone-based energy.
Through strategies like:
Therapeutic ketogenic diets
Glutamine inhibition
Fasting and calorie restriction
Hyperbaric oxygen therapy
It may be possible to disrupt the metabolic foundation that glioblastoma depends on, improving outcomes and quality of life—especially when used alongside standard care.
This isn’t about false hope or magic bullets. It’s about giving patients another tool—one rooted in rigorous science and metabolic common sense.
Resources
Disclaimer:
The information provided in this blog, podcast, and associated content is for educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. The content shared is based on reputable sources, medical literature, and expert insights, but it should not be used as a replacement for direct consultation with a licensed healthcare provider.
No Doctor-Patient Relationship: Engaging with this content does not create a doctor-patient relationship between you and QuickLabMobile or any contributors. Always consult with a qualified physician, specialist, or healthcare professional before making any medical decisions, changing your treatment plan, or starting/stopping any medications.
Not a Substitute for Medical Advice: While we strive to provide accurate and up-to-date information, medicine is constantly evolving. New research, treatments, and medical recommendations may emerge, and individual health conditions can vary. Do not rely solely on this content for health decisions. If you are experiencing symptoms, have concerns about your health, or require medical assistance, seek immediate care from a licensed medical professional.
Emergency Situations: If you are experiencing a medical emergency, such as difficulty breathing, chest pain, signs of a stroke, or any other life-threatening condition, call 911 (or your local emergency services) immediately. Do not delay seeking emergency care based on information provided here.
Liability Disclaimer: QuickLabMobile, its contributors, and any associated entities do not assume liability for any damages, harm, or adverse outcomes resulting from the use, interpretation, or misuse of the information provided in this content. You are responsible for your own healthcare decisions and should always verify information with a trusted medical professional.
External Links & References: This content may include links to external sources, medical studies, or third-party websites for further reading. These links are provided for convenience and informational purposes only. QuickLabMobile does not endorse, control, or take responsibility for the accuracy of external content. Always verify information with authoritative sources such as the CDC, NIH, WHO, or Mayo Clinic.
Final Note: Your health is unique, and what works for one person may not be suitable for another. Stay informed, ask questions, and always prioritize professional medical guidance.


